Beginning on January 1, 2025, members who are covered under the nationally negotiated railroad health & welfare plans will have their pharmacy benefits transitioned from Express Scripts, Inc., to Optum Rx. This includes H&W Plan numbers GA-690100 (SMART-TD Plan), GA-23000 (National Railroad Plan), and GA-46000 (Early Retiree Plan).
Tag: GA-23111
UnitedHealthcare has announced that enrollment is open under Group Policy GA-23111.
From November through December 2018, any individual who is eligible for coverage under one of the GA-23111 plans can enroll and will be accepted for coverage without any medical underwriting or requirement of good health. This includes family members who may not already be covered by the policy.
There are no limitations for pre-existing conditions, and coverage will be effective Jan. 1, 2019.
Only applicants whose completed enrollment forms are postmarked in November or December 2018 will be considered for enrollment.
This enrollment is for former railroad employees (and their dependents) who:
- Were previously covered under any railroad health plan and were represented by a railway labor organization, or
- Were members in accordance with the constitution or bylaws of one of the participating railway labor organizations when coverage under their applicable group health plan ended.
Open enrollment under Plan F is available for railroad employees’ parents or parents-in-law who are eligible under Medicare.
For persons eligible for Medicare, call 800-809-0453 for more information.
For persons not eligible for Medicare, call 800-842-5252 for more information.
To get an enrollment form, visit www.yourtracktohealth.com and follow the “Plan Your Retirement” link at the top of the home page, then visit “Essential Forms” and then “Group Policy GA-23111 Enrollment Form.”
A PDF with more information about GA-23111 is available for download.
An open enrollment period for GA-23111 Plan E also is underway in November and Decemeber.
GA-23111 Plan E is made available by rail labor organizations and pays 70 percent on eligible expenses of the 20 percent not covered under GA-46000, which is the Railroad Employees National Early Retirement Major Medical Benefit plan (ERMA). Combined, GA-46000 and Plan E cover 94 percent of your eligible expenses.
- Plan E has a $100 calendar year deductible per individual.
- Plan E adds an additional lifetime maximum amount of $500,000 for you and each enrolled dependent, which is much higher than for GA-46000 alone
- Plan E has some benefits for routine and/or preventive benefits. For example, covered expenses for pap smears and mammograms are payable in full at 100 percent and not subject to the calendar year deductible. However, the charge for the office visit in connection with the preventive service is not payable under Plan E.

There are no limitations for pre-existing conditions. Enrollment in November and December 2014 will be for coverage effective Jan. 1, 2015. Only those applicants whose completed enrollment form is postmarked in November 2014 or December 2014 will be considered for open enrollment.
This open enrollment is being held for former railroad employees (and their dependents) who:
- Were previously covered under any railroad health plan and were represented by a railway labor organization or,
- Were members in accordance with the constitution or by-laws of one of the participating railway labor organizations, when coverage under their applicable group health plan ended.
If someone you know meets these GA-23111 eligibility provisions, open enrollment provides an opportunity for them to become covered. Other eligible members of your family may also enroll if they are not currently covered. In addition, open enrollment under Plan F is available for railroad employees’ parents or parents-in-law who are eligible under Medicare.
Anyone interested in enrolling should call one of the following phone numbers to get additional information about these plans:
- For persons eligible for Medicare, call (800) 809-0453;
- For persons not eligible for Medicare, call (800) 842-5252.
Visit YourTracktoHealth.com to download an enrollment form and view plan rates.
During November and December, UnitedHealthcare will hold an open enrollment under railroad plans GA-23111.
During this open enrollment period, any individual eligible for coverage under one of the GA-23111 plans may enroll and be accepted for coverage without medical underwriting or requirement of good health.
There are no limitations for pre-existing conditions.
Enrollment in November and December is for coverage effective Jan. 1, 2011.
Only those applicants who mail their completed enrollment forms in November or December will be considered for open enrollment.
The next opportunity to enroll during an open enrollment period will not be until November 2012, consistent with the plan’s two-year open enrollment cycle.
This open enrollment is:
- For those covered under any railroad health plan and represented by a railroad labor union.
- For those who are members in accordance with the constitution or bylaws of one of the participating railroad labor unions when coverage under the employer group health plan applying to them ends.
If you, or someone you know, meets the GA-23111 eligibility provisions, open enrollment provides an opportunity to become covered.
You may also enroll your spouse or eligible children if they are not currently covered. In addition, enrollment under Plan F is available for your parent or parent-in-law. Anyone interested in enrolling should call one of the following phone numbers to obtain an enrollment form or additional information:
- For persons eligible for Medicare, call (800) 809-0453.
- For persons NOT eligible for Medicare, call (800) 842-5252.
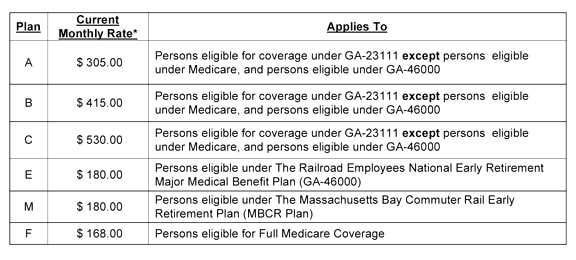
Note: Enrollment during November and December of the open enrollment period provides for coverage effective the following calendar year, Jan. 1 through Dec. 31. Each June 1 of that calendar year, and only at that time, adjustments to the premium for all plans under GA-23111 may occur. Additionally, if you are enrolled in either Plan A, B or C under GA-23111, and a change in the premium amount you pay does occur, you will be allowed, at that time, to switch your plan to a different plan (A, B, or C) with a lower premium, if available.
Here’s an opportunity to save a 44-cent stamp and better assure your UnitedHealthcare payments for GA-23111 plans and COBRA coverage arrive on time.
It’s called electronic funds transfer, or EFT, and it permits your UnitedHealthcare premiums for GA-23111 plans and COBRA coverage to be automatically deducted from your checking account, even when you are away from home.
Using EFT, says UnitedHealthcare, provides peace of mind that your insurance premiums reach UnitedHealthcare on time and that you always will pay the proper rate and that the proper amount will be deducted from your checking account.
Your EFT payments will show up on your bank statement.
To sign up with UnitedHealthcare for EFT:
- Print out and complete the downloadable form provided below, and sign it.
- Attach a void check.
- Send the completed and signed form, with the voided check, to:
You should continue making your monthly payments by check until notified that your monthly automated withdrawal will occur. You will receive a “verification of electronic premium withdrawal” statement, which will replace the monthly billing statement. The statement will advise the date when the withdrawal will take place and the amount to be withdrawn.
Also, premiums must be paid through the current period in order to enroll.
Answers to questions can be obtained by calling UnitedHealthcare at (800) 842-5252.
Click here for the enrollment form.